Visit the Evidence Files Facebook and YouTube pages; Like, Follow, Subscribe or Share!
Find more about me on Instagram, Facebook, LinkedIn, or Mastodon. Or visit my EALS Global Foundation’s webpage here.
The Situation
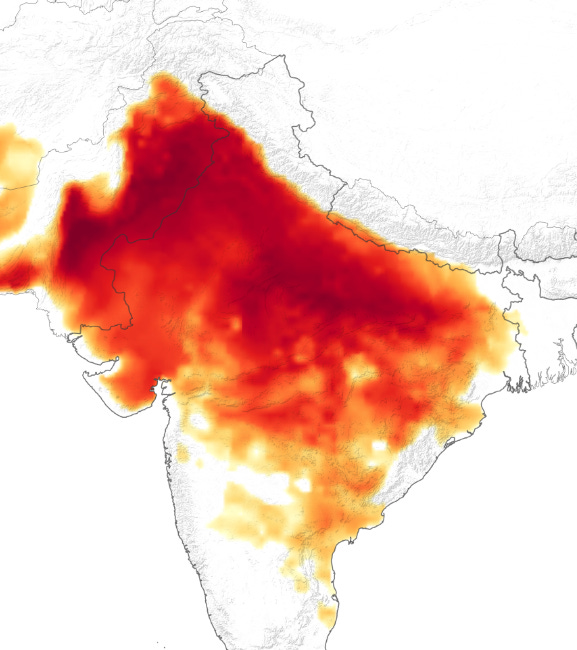
Seventeen species of venomous snakes call Nepal home. Snakes produce venom primarily for hunting, but often use it for self-defense. Curiously, little research exists that examines the evolution of snake venom as a mechanism of defense, despite more than 2 million bites globally on humans, and an average of 80,000 to 100,000 people dying annually from defensive bites. This dearth of research is partly why the development of a sufficient and affordable number of antidotes remains a complex, and often mystifying endeavor. As researcher José María Gutiérrez and team point out, “The composition of snake venoms shows high complexity and diversity, resulting in a variable biochemical and toxicological profile that determines a wide range of clinical manifestations.” According to the National Guidelines for Snakebite Management in Nepal, Nepal possesses just one antivenom, imported from India. This antivenom is polyvalent, meaning it is effective against four common species of snakes found in India and Nepal: Russell's Viper (Daboia russelii), Common Cobra (naja naja), Common Krait (Bungarus caeruleus) and Saw Scaled Viper (Echis carinatus). Unfortunately, the guidelines report that the antivenom is “costly and scarce.”
Russell's Viper (Daboia russelii); source: Wikimedia Commons
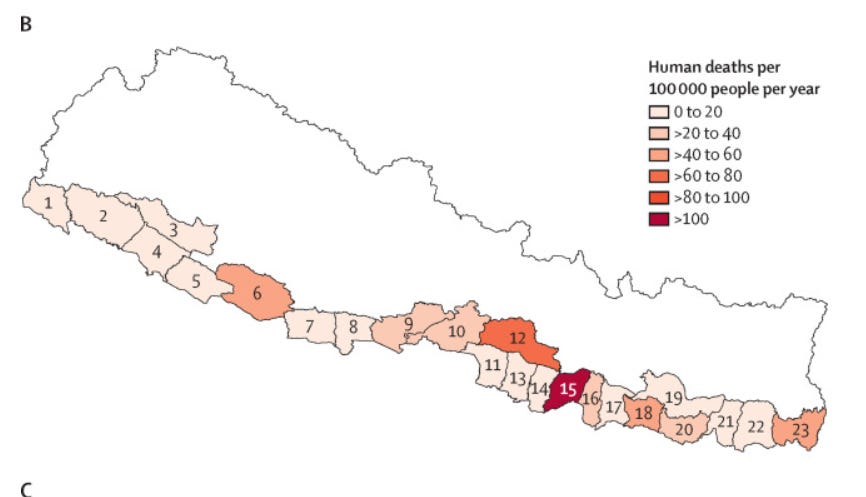
In 2022, the Kathmandu Post called snakebites in Nepal “an invisible neglected crisis.” It stated that up to 3,000 people die per year, almost all in the Tarai region. A report in the Lancet found that of the people bitten and envenomed there, approximately 7 to 8% succumbed to the venomous effects. Females and children were disproportionately affected both in number of bites and mortality from them. And these numbers are probably lower than the actual. Dr. Sanjib Kumar Sharma, a snakebite expert at the World Health Organization, told the Kathmandu Post that “A lot of people bitten by venomous snakes die before reaching hospitals.” This circumstance often skews the official record maintained by the Health Ministry according to spokesperson Dr. Samir Kumar Adhikari, who previously served as chief of the Zoonotic Section at the Epidemiology and Disease Control Division. “Those who die before reaching health facilities do not come in our record,” he stated. This deficiency in reporting happens in many countries where snakebites occur most frequently in rural areas. The WHO estimates about 40% of deaths from snakebite envenomation happen within villages, 40% happen during transport to treatment centers, and only 20% of deaths occur in hospitals. In addition to a probably higher number of deaths by snakebite, these facts suggest that some people do not or cannot seek appropriate treatment, cannot make it to a medical facility quickly enough when they do, or the hospitals available to them simply do not possess the necessary antivenom to save their lives.
Before discussing the situation in Nepal more closely, here is an explanation of how snake venom generally works.
Snake Venom Physiology
Researchers set out to determine whether there is in fact a functional difference between a snakebite geared toward predation versus one focused on self-defense. Answering this question could help in the development of antivenoms. Bangor University researcher Harry Ward-Smith created a questionnaire centered on a particular question—what is the timescale of pain effects from a venomous snakebite? Why study this metric? Scientists believe that venom used specifically for defense should necessarily create an acute pain reaction thereby discouraging the potential predator from continuing to pursue the snake. As Smith et. al. wrote:
Bee stings hurt. So do wasp stings, scorpion stings, the bites of centipedes, and the venom injections of many other animals, including snakes. To inflict pain is not necessarily to the advantage of an animal that uses its venom strictly for incapacitation of prey. In fact, it may be to its disadvantage because pain may induce increased struggling on the part of the prey. But venoms are also used defensively, and it is in that context that they may derive their effectiveness largely, if not exclusively, from their pain-inducing qualities. It is principally because venoms are painful that they can function in defense.
In many venomous snakebites, Smith’s team noted, sufferers feel little to no pain often until other effects commence that themselves cause pain. People who receive bites in these circumstances typically endure critical effects from the venom well before they know they have been poisoned or are aware of the severity of their condition. Determining whether defensive venom functions differently than that for predation purposes might inform the development of more effective and efficient antivenoms, because once the venom sets to work on a victim’s internal systems the destruction is swift and severe.
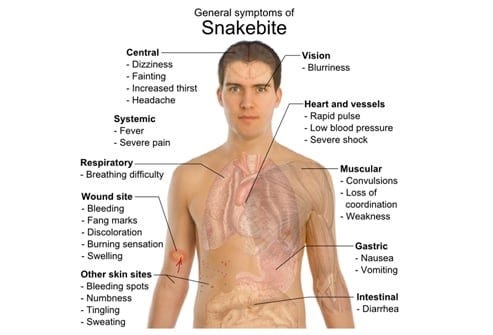
Depending on the breed of snake and its associated venom, victims can endure any number of horrific maladies, such as:
chronic morbidity, disability and psychological sequelae including,
amputations;
post-traumatic stress disorder;
blindness;
maternal and fetal loss;
contractures (that is, permanent shortening of a muscle or joint that often leads to deformity or rigidity); or
chronic infections and malignant ulcers
Snake venoms consist of various protein mixtures that can act individually or as an “integrated phenotype.” Among different species, the composition and subsequent effects of venom vary significantly. Grappling with these variations in order to create antivenoms has evolved into its own field called “antivenomics.”
Researchers note that even the delivery system differs among species. Depending upon the fang size, snakes inject venom either subcutaneously or intramuscularly. Subcutaneous delivery (just below the outer skin) can lead to localized effects on neighboring tissues, while intramuscular injection allows passage of the venom through the lymphatic or circulatory systems. Local tissue damage occurs from myotoxic phospholipases binding to and disrupting muscle fiber membranes. Toxins distributed this way cause degenerative effects on the victim cells leading to irreversible muscle cell damage, in some cases including muscle contracture and necrosis. This kind of destruction on muscle membranes then invokes considerable pain among victims. Some venoms employing this method of devastation also damage blood vessels, starting with distension and eventually leading to extravasation, or the seeping of blood from the vessel into the body (i.e., internal bleeding).
Other venoms contain neurotoxicity traits, meaning they bind to cholinergic receptors. These receptors perform various critical functions, such as controlling the involuntary mechanisms of organs (how a person breaths or the heart beats without conscious thought or effort), or allowing instructive transmissions to pass along the nervous system to the appropriate body part (which is how a person moves). Neurotoxic venom inhibits these processes causing intracellular degeneration, ultimately destroying the nerve terminals. Patients then suffer long-term or permanent paralysis that can cover large areas of the body. In other cases, such neurotoxicity causes involuntary contractions in various muscle groups, which can inflict extraordinary pain or restrict critical bodily functions such as breathing. Some venoms assault the cardiovascular system directly. Doctors often see bleeding from organs in patients affected by these types. Results might include ischemia, stroke, or neurological sequelae—the latter causing all kinds of maladies from kidney failure to aphasia or paralysis. In other cases, the venom provokes coagulation—thickening of the blood—which can cause defibrination. Defibrination leads to all kinds of horrific consequences including, ultimately, death.
Source: Medscape
Snakebite Victims and Mitigations in Nepal
Having only summarized the various effects a snake bitten person might suffer, it is clear why victims need rapid, comprehensive care. A primary issue for some in Nepal is that snakebites often do not hurt that badly, so the seriousness of the consequences remain elusive for a while. By then, it is too late for some. Almost all reported venomous snakebites in Nepal occur in the Tarai, particularly in the Eastern and Central regions, but these areas remain largely underserved by medical facilities capable of treating them. (Snakebites do occur in the hills and mountain regions, as there are 10 venomous species calling those areas home. To date, however, no comprehensive analysis has been done to determine the number of bites and the rates of serious injury or morbidity in those regions. For more on this, see this study). Unsurprisingly, victims who receive immediate treatment, particularly with antivenom or ventilation, enjoy far better outcomes than those who do not. Nearly 20% of all patients require surgical intervention, and those who saw the snake that bit them tend to receive more effective treatment because that knowledge allows doctors to use more targeted medical procedures.
Credit: Snakebite epidemiology in humans and domestic animals across the Terai region in Nepal: a multicluster random survey
The two highest risk factors contributing to the probability of humans enduring a bite by venomous snakes in the Nepal study were 1) storing straw and 2) having households of five or more people. Bites most frequently targeted lower limbs, indicating that incidents typically resulted from victims stepping on or very near the snake. Nearly 30% of all victims suffered some severe affect (among those described above); of these the cobra and krait appeared to inflict the most bites of any species. For those people who suffered envenoming, only half received antivenom. These patients died or suffered permanent injuries in far lower numbers than those who did not receive an antidote. Even those who recovered, though, indicated a high prevalence of PTSD, highlighting the need for psychological intervention as well as medical. Children ages 4 to 15 years old suffered the highest mortality rate, primarily because smaller doses of venom inflict upon them the same level of trauma as adults (and no evidence conclusively suggests that snakes can or do measure/limit their distribution volume based on the size of their target). In other words, the toxicity of a bite to children is many times higher than a bite to an adult, and therefore more likely to be severe or fatal. Moreover, females died at inordinate rates compared to males, comprising as much as 73% of all fatalities or permanently disabling injuries in adults.
Several mitigation measures are available to people living in snakebite-prone areas. A key aspect to this, like anything, is education. Dr. Krishna Bohara of Seti Zonal Hospital told the Kathmandu Post, “In rural areas, people still approach witch doctors. If you don’t get well there, they then come to the hospital.” That delay in receiving medical care may make the difference in a positive, negative, or fatal outcome. In other cases, people follow traditional treatments, which also causes delays in receiving proper care or prevents it altogether. And yet in other instances, people adopt more superstitious approaches. For example, some believe that killing the snake that bit them will prevent any negative affect from the venom.
Kraits, the species most frequently associated with bites in the Tarai, typically attack people working in farm fields or around the home. Educating farm workers on how to take measures in response to this potential scenario can be life saving. For example, wearing shoes and pants reduces the risk factor by some small amount. This requires checking them before putting them on. Around the home specifically, clearing high grasses, straw, and other items snakes can use to hide in has shown to lower snakebite incidents in many areas of the world. The presence of rats and mice increases the chances of a human-snake encounter as the serpents feed on these creatures in abundance; and rodents tend to proliferate in places with an excessive number of hiding spots. Keeping livestock away from the home and taking other action to minimize the population of rodents in and around the household greatly lowers the possibility of a snakebite. Adopting precautions in the monsoon season especially would mitigate risk, as that time of year leads to higher numbers of human-snake interactions as the snakes alter their feeding behavior and movements. In addition to the above mitigations, removing dry hiding places for snakes during the monsoon tends to discourage them from sticking around. Sleeping under mosquito nets or at least off of the ground also reduces the incidents of bites.
The Rufford Foundation started a campaign in 2020 in Nepal and India with both conservation and education about snakes as its primary focus. It describes it this way:
Snakebite is a life-threatening public health problem in Nepal and many people kill snakes on sight because of the fear of being bitten…. and snakebite victims use inappropriate and harmful first aid methods which increase human-snake conflicts in communities. There are a lot of misconceptions and traditional beliefs about snakes and snakebites which provokes people to kill the snakes when they are encountered. We suspect some unscientific and wrong messages in social media may also stimulate people to kill snakes… [T]o minimize all the unscientific and unnecessary activities and also to spread awareness and to build capacity of the local people in a larger scale, we designed this project "Education in Motion: Strategies to Engage Communities in Snake Conservation When Science isn't Enough."
Click below to see their educational video.
Antivenom Production
“Anti-venom is complicated. It's hard to manufacture. It needs to be refrigerated. And it's snake-specific,” Amanda Aronczyk of NPR correctly pointed out. Indeed, the complexity of manufacturing, the variety of antidotes to manufacture, and the fragility of them make it a costly and tenuous solution to areas of abundant snakebites. Nevertheless, such antivenoms remain the only accepted clinical treatment. In response to the challenges of developing affordable mass-produced antivenom, researchers have examined alternatives incorporating “bioactive compounds isolated from plant extracts with different properties such as analgesic, anti-myotoxic, anti-hemorrhagic, and anti-inflammatory effects.” Some alternatives to antivenom are used in the United States that target particular functions of venom associated with specific indigenous species of snakes, but these come with their own side-effect risks and are not wholly effective, nor are they considered a clinical alternative to antivenom. Moreover, many of these treatments themselves are expensive, which makes them all but unavailable to places like Nepal.
Traditional doctors in rural areas have long employed certain plant extracts to counteract the effects of venom. Scientific studies have shown the efficacy of some of these substances in inhibiting or slowing some venomous effects. Unfortunately, few studies have tested these extracts’ inhibiting effects and their molecular components for use in mass-producing medicinal treatments. Scientists nonetheless are working on the problem. As Isabel Gómez-Betancur, et. al. note:
New and much improved antivenoms with high standards can be produced in adequate volumes when multidisciplinary, international collaborative efforts are undertaken. This would help serve not a particular nation but entire regions… It is important to take advantage of new biotechnological approaches for the development of new antivenoms. These could be based on mixtures of human monoclonal antibodies that could directly replace the polyclonal equine antibodies that are currently being used in conventional antivenoms.
For now it seems the status quo reigns, but hope looms on the horizon.
Conclusion
Individual efforts at mitigation would undoubtedly help reduce the numbers of fatalities or severe injuries, but these are not a panacea. The Tarai region’s economy relies heavily on agriculture. Current farming methodologies place tens of thousands of people within the same physical space as the snakes that pose the greatest threat. For the present at least, humans are going to be bitten regardless of the precautions they take. What’s needed then, is a more robust production and distribution network for antivenoms. As noted, they currently remain “costly and scarce.” One silver lining, however, is that the vast majority of lethal snakebites in Nepal come from just two species of snakes. This allows experts and authorities to prioritize just one or two antivenoms. Perhaps an enterprising Nepali scientist will find a way to develop this limited number of antidotes in an inexpensive way at the needed volume. The culture of the Tarai is one of community, so if antivenom becomes widely available and affordable, I predict its distribution would be handled in an effective manner by employing the community’s participation. Indeed, Dr. Sanjob Sharma showed precisely how this could work. In a study he conducted about a decade ago, he was able to reduce the case-fatality rate of snakebites from 10.5% to 0.5% during his intervention in which researchers educated locals on mitigating snake encounters and provided rapid transport for bitten victims via motorcycles.
Photo by: Dr. Sanjib Sharma, sourced from the Kathmandu Post
As I have reported in previous pieces on environmental issues, when stakeholders take control of the situation, things tend to get done. Solving the problem of the developmental costs and complexity of antivenom is, in my view, the key to foreclosing the “invisible neglected crisis” of snakebite deaths and disability in Nepal. Once that happens, I have every confidence affected communities will see to the rest.
Common Cobra: Photo by: Dr. Sanjib Sharma, sourced from the Kathmandu Post
***
I am a Certified Forensic Computer Examiner, Certified Crime Analyst, Certified Fraud Examiner, and Certified Financial Crimes Investigator with a Juris Doctor and a Master’s degree in history. I spent 10 years working in the New York State Division of Criminal Justice as Senior Analyst and Investigator. Today, I teach Cybersecurity, Ethical Hacking, and Digital Forensics at Softwarica College of IT and E-Commerce in Nepal. In addition, I offer training on Financial Crime Prevention and Investigation. I am also Vice President of Digi Technology in Nepal, for which I have also created its sister company in the USA, Digi Technology America, LLC. We provide technology solutions for businesses or individuals, including cybersecurity, all across the globe. I was a firefighter before I joined law enforcement and now I currently run a non-profit that uses mobile applications and other technologies to create Early Alert Systems for natural disasters for people living in remote or poor areas.







How scary to be around so many snakes that can kill you and only a fraction of different Anti-Venom to save you.. or going blind or amputations .. terrifying realities. What area of the body is usually bitten?